Lung cancer is the uncontrolled growth of abnormal cells originating within the lungs, usually in the layers of cells that line the air passages. These abnormal cells do not go through the natural stages of growth, division, and dying that normal cells do. They divide unchecked, often forming one or more masses of cells (tumours). Tumours can damage healthy tissue and grow large enough to interfere with breathing. Lung cancer can eventually spread (metastasize) beyond the lungs into nearby lymph nodes, tissues, and other organs.
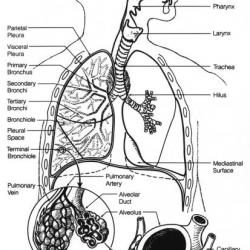
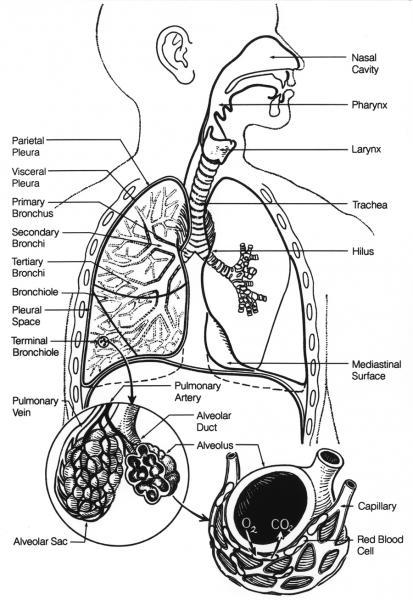
The lungs are part of the respiratory (breathing) system and are located in the chest, inside the rib cage and above the diaphragm. When a person inhales, air enters the lungs and flows through passages of decreasing diameter called bronchi and bronchioles. These passages carry oxygen to small sacs (alveoli) deep within the lung, where oxygen moves from the lung into the bloodstream, and carbon dioxide, a by-product of metabolism, moves from the blood into the lung to be exhaled. Any lung disease that interferes with this exchange process, including lung cancer, can limit the amount of oxygen available and affect tissues and organs throughout the body.
According to Cancer Research UK, lung cancer is the third most common cancer in both men and women and accounts for more than a fifth of all cancer deaths. Cancer Research UK estimates that in 2014 there was 46,403 new cases of lung cancer and 35,895 deaths from lung cancer.. While anyone can get lung cancer, about 4 out of 10 new cases will be in people 75 years of age or older.
Risk factors for developing lung cancer include:
- Smoking – at least 86% of lung cancer deaths are thought to be related to smoking. The more a person smokes, and the longer that he or she smokes, the greater the risk. Second-hand smoke also increases risk of lung cancer.
- Asbestos exposure – this can increase the risk of lung cancer, related to 6-8% of cancer cases. Asbestos is more commonly associated with mesothelioma, a rare cancer of the lining of the chest and abdomen. Most cases of mesothelioma – about 70% to 80% – arise in people with a history of working with asbestos, especially in the shipbuilding, construction, automotive, and fireproofing industries.
- Rarely other factors may contribute such as occupational exposure to cancer-causing substances (carcinogens) e.g. arsenic, chromium, or air pollution (diesel engine exhaust), exposure to radiation (such as previous treatment for another type of cancer) or genetic factors where there is a family or personal history of lung cancer.
Lung cancer begins in one of the cell types that exist in the lungs. Most cases are thought to be due to an acquired genetic change or mutation in DNA that leads to the production of an abnormal protein that either promotes the uncontrolled growth of cells or inhibits their natural death.
Cancer that spreads from another part of the body to the lungs, such as metastatic breast cancer, is not considered lung cancer. Cancers that have spread to the lungs, sometimes called secondaries, from other areas are treated differently, such as according to the cancer type of origin (the primary).
There are two main categories of lung cancer, non-small cell and small cell. These cancers are named and differentiated based upon the size, shape, and characteristics of the tumour cells. Non-small cell lung cancer (NSCLC) is the most common type with several different varieties based on histological appearance (how the cells look down a microscope). NSCLC types include tumours common to both smokers and non-smokers. Small cell lung cancers (SCLC) are rarer and are most commonly, but not exclusively, seen in smokers. In addition, there are several much rarer types of lung cancer e.g. carcinoid and sarcoma.
There are no UK data on survival from specific types of lung cancer. In 2007 a worldwide study, including 19 countries, called the Lung Cancer Staging Project showed survival differences based on stage of lung cancer (how advanced it was on presentation) and type. Stage 1 NSCLC had, at best 73% of people alive after 5 years, with 13% alive at 5 years with stage 4 cancer. For SCLC 40% of people were alive after 5 years with stage 1 and 1% alive at 5 years with stage 4 cancer. It is likely that these figures have changed in the intervening years, particularly with new treatments available.