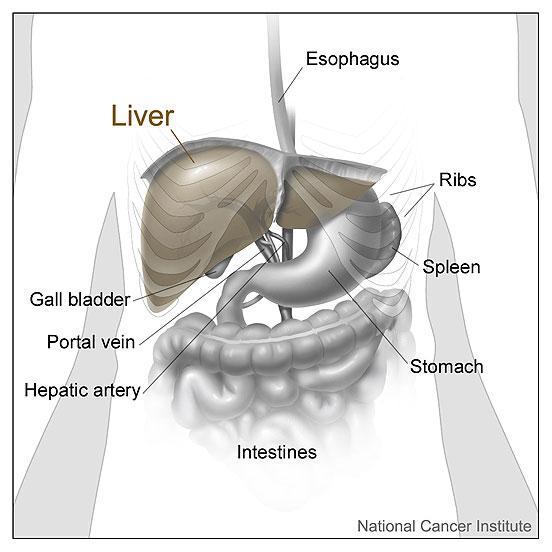
The liver is a vital organ located in the upper right-hand side of the abdomen. It performs numerous functions for the body: converting nutrients derived from food into essential blood components, storing vitamins and minerals, regulating blood clotting, producing proteins and enzymes, maintaining hormone balances, and metabolising and detoxifying substances that would otherwise be harmful to the body. The liver also makes factors that help the human immune system fight infection, removes bacteria from the blood, and makes bile, which is essential for digestion.
Bile, a greenish-yellow fluid consisting of bile acids (or salts) and waste products, such as bile pigments, flows through small bile ducts inside the liver. The bile flows from these small ducts into larger ones, like streams into a river, eventually leading to the common bile duct. The cystic duct connects the common bile duct to the gallbladder. After eating, the gallbladder, an organ that sits next to the liver and stores bile, releases bile into the small intestine where it helps to digest fats.