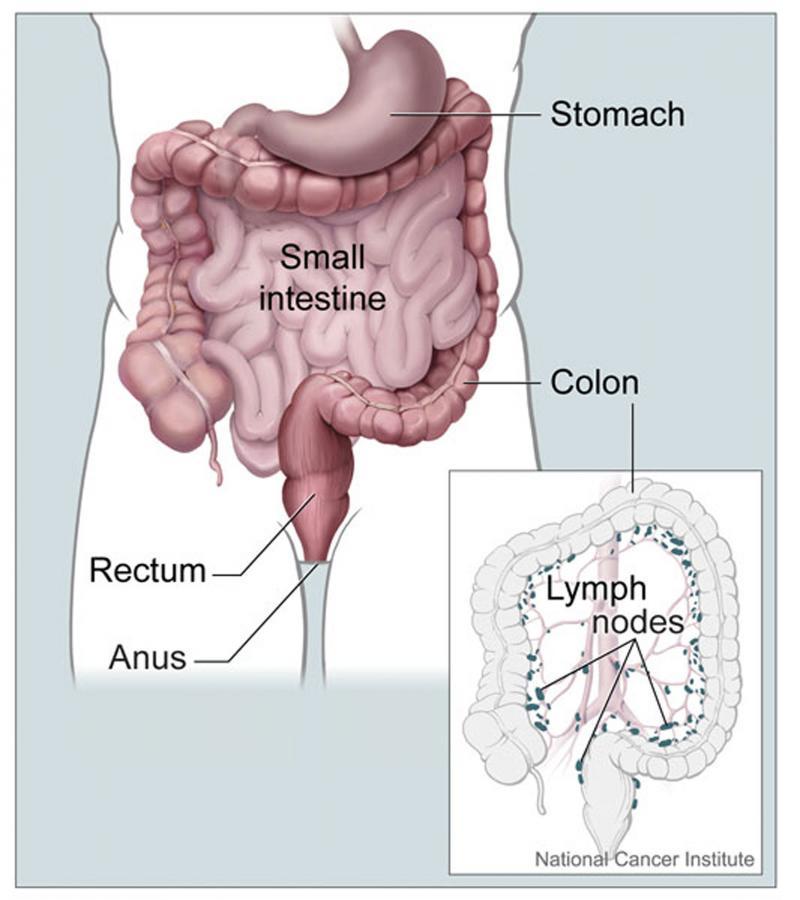
Inflammatory bowel diseases (IBD) are chronic disorders affecting more than 300,000 people in the UK. The disorders are characterised by inflammation in the lining of the intestine.
Inflammatory bowel disease is not the same as irritable bowel syndrome (IBS). IBS is a more common condition that causes symptoms such as bloating, abdominal discomfort, and change in bowel habits (diarrhoea and/or constipation). IBS is not associated with inflammation or change in structure of the bowel.
The cause of IBD is not known, but are thought to be due to an autoimmune process where the immune system starts attacking the individual’s healthy gastrointestinal tract tissue.
IBD affects slightly more women than men and is seen most frequently in Caucasians. Other common risk factors which increase the risk of developing IBD include use of nonsteroidal anti-inflammatory medications (NSAID), e.g. Ibuprofen, and smoking.
The most common inflammatory bowel diseases are Crohn’s disease and ulcerative colitis. In the UK, ulcerative colitis is twice as common as Crohn’s disease. Both diseases can start at any age, but the majority are first diagnosed in patients between the ages of 15 and 40 and a smaller number between 60 and 80. Children affected by either disease may experience delayed growth and development, in addition to gastrointestinal symptoms e.g. abdominal pains.