Task Force Issues New Guidelines for Taking Cholesterol-Lowering Statins
The U.S. Preventive Services Task Force (USPSTF) recently updated its 2008 guidelines on cholesterol-lowering medications known as statins. The recommendations were released in the November 15th issue of the Journal of the American Medical Association.
The main recommendations apply to all adults ages 40 to 75 with no history of heart disease but with at least one risk factor, such as smoking, high cholesterol, high blood pressure or diabetes, and a 10% or greater risk for a heart attack or stroke in the next ten years based on the American College of Cardiology/American Heart Association risk calculator. The task force now advises these adults to take a low or moderate dose of a statin drug every day.
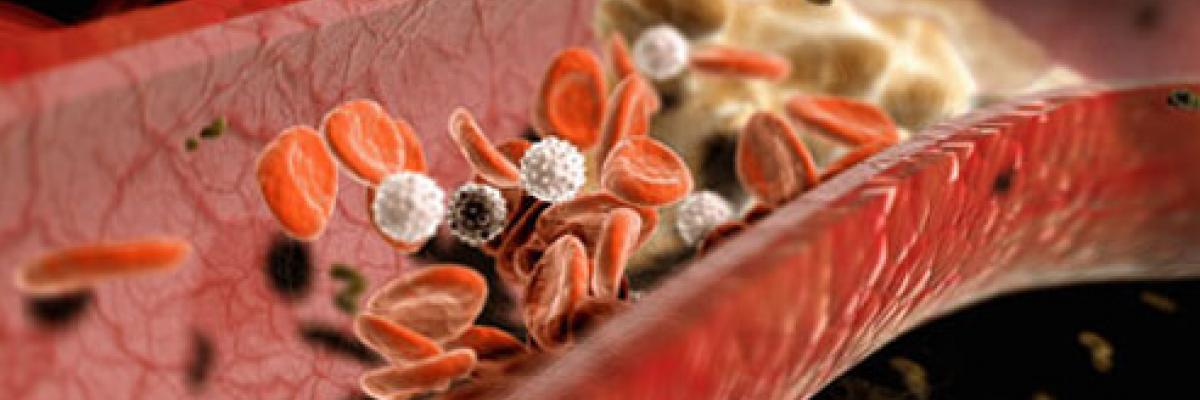
In the U.S., cardiovascular disease (CVD) is the number one cause of death in both men and women, accounting for 1 in 3 deaths from heart attacks and strokes. Statins work to lower risk of CVD by reducing the production of cholesterol in the liver, lowering low-density lipoprotein (LDL; the "bad" cholesterol) and triglycerides in the blood while raising high-density lipoprotein (HDL; also known as "good" cholesterol). In addition, statins may also help to lower CVD risk by reducing inflammation and stabilizing plaques in blood vessel walls.
In a recent interview for Stanford University, Douglas Owens, MD, a Stanford professor of medicine and member of the task force when the guidelines were developed, said that the task force's recommendations previously focused on screening for high cholesterol rather than on statin use. The new guidelines now advise healthcare practitioners and their patients to go beyond screening for high cholesterol and to evaluate a person’s overall risk for CVD to determine who may benefit from statins.
"The accumulating evidence on the role of statins in preventing heart disease has now led the task force to reframe its main clinical question from 'Who should be screened for [high cholesterol]?' to 'Which population should be prescribed statin therapy?'," said Dr. Owens. The USPSTF made its decision by reviewing 19 clinical trials that included more than 73,000 patients. Based on that review, the task force determined that, although statins can produce side effects such as muscle pain, and, in rare cases, liver failure, and may be a risk factor for diabetes, the benefits of taking the drugs outweigh the risk for those people who have an increased risk of a stroke or heart attack.
For people with at least one risk factor for CVD and a risk of 7.5% to 10% for heart attack or stroke based on the calculator risk assessment, the task force recommends a conversation between the patient and his or her healthcare practitioner on whether or not to take statins. The task force didn't find enough evidence to suggest starting people 76 and older on statins. However, an editorial published in JAMA in the same issue as the new guidelines says, "[I]t is not necessary to stop statin therapy when a 75-year-old turns 76."
Research is continuing on both the benefits and side effects of statins. Some patients and healthcare practitioners may choose not to use the drugs, especially if side effects such as muscle pain and weakness become intolerable. In a press release issued by the task force, Dr. Owens says that, "Regardless of your risks for heart disease, everyone can benefit from not smoking, eating healthy, exercising, and limiting alcohol use. Statins aren't always the answer. Talk to your doctor about whether taking a statin to help prevent heart disease is right for you."

