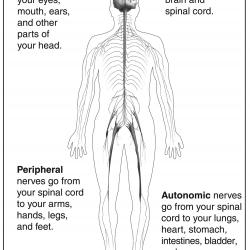
Neuropathy is any disease or disorder that affects the functioning of nerves in a person's body. The nervous system is divided into two parts, the central nervous system (CNS), which includes the brain and spinal cord, and the peripheral nervous system, which branches off from the brain stem and spinal cord to the rest of the body. The peripheral nervous system is further subdivided into the somatic and autonomic nervous systems. The somatic nervous system controls sensation and movement, while the autonomic nervous system controls vital functions, such as heart rate and breathing.
Nerve cells originate in the central nervous system and have long fibres that extend throughout the body and terminate as nerve endings in skin, muscle, and organs. These cells transmit impulses from the brain and spinal cord to other parts of the body.
- Sensory nerves relay information about temperature, pressure, vibration, pain, and muscle position from various locations in the body (such as the tip of an index finger) to the brain.
- The brain processes impulses from sensory nerves and also sends commands to muscle groups through motor nerves, allowing someone, for example, to walk, sit, run, and grasp objects.
- Autonomic nerves send and receive messages that affect internal organs and involuntary functions, such as regulating blood pressure and heart rate, breathing, and digestion.
Neuropathy can develop in a wide variety of diseases and conditions. It may be inherited or acquired, acute or chronic, temporary or permanent. Nerve damage may occur in a single location or may be widespread. It may affect primarily one type of nerve, such as sensory, or multiple types. Anything that damages nerves can interfere with their ability to transmit accurate signals, which can lead to a number of signs and symptoms.
Neuropathy can affect both the central and peripheral nervous systems, this article will focus mostly on peripheral neuropathy, with some discussion of autonomic neuropathy. Peripheral neuropathy is a relatively common condition that affects around 1 in 50 people in England, with 8% of people who are 55 years of age or over being affected by it.