To help diagnose or rule out a phaeochromocytoma or other neuroendocrine tumour
Urine Metadrenalines (Metanephrines)
When you have symptoms of increased catecholamine release, such as persistent or episodic high blood pressure, severe headaches, rapid heart rate, and sweating.
Foods such as coffee (including decaffeinated), tea, chocolate, vanilla, bananas, oranges and other citrus fruits should be avoided for several days prior to the test and during collection. There are also many medications that can potentially affect test results. Talk to your doctor about any prescriptions and over-the-counter drugs and supplements that you are taking. Wherever possible, those that are known to interfere should be discontinued prior to and during sample collection. Emotional and physical stresses and vigorous exercise should be minimised prior to, and during, test collection as they can increase catecholamine secretion.
-
How is it used?
Urine metadrenaline testing is mainly used to help detect and rule out phaeochromocytomas in patients with symptoms. Urine metadrenaline testing may be requested by itself or along with a plasma metadrenalines test. Plasma or urine catecholamine testing may also be requested, either along with urine metadrenalines or as follow-up tests. Since catecholamine secretion tends to vary during the day, a 24 hour urine test for metadrenalines or catecholamines may detect excess production that is missed with a blood test. It is up to your doctor to decide which test or test combinations will provide the most information. In many cases, urine or plasma metadrenalines may be preferred as they are usually present in greater quantities than catecholamines in the urine and can persist in the blood even when catecholamine levels have returned to normal.
Since these tests are affected by drugs, foods, and stresses, false positive tests may occur. For this reason, metadrenaline testing is not recommended as a screen for the general public. Doctors will frequently investigate a positive result by evaluating a person's stress, diet, and medications, working to alter or minimise these influences, and then repeating the test to see if the changes have been effective.
Occasionally, metadrenaline testing may be requested for an asymptomatic person if a possible adrenal or neuroendocrine tumour is found on a scan that is done for another purpose (called an incidentaloma) or if the person has a strong personal or family history of phaeochromocytomas (as they may recur and there is a genetic link in some cases).
-
When is it requested?
Urine metadrenalines are requested when a doctor either suspects that someone has a phaeochromocytoma or wants to rule out the possibility. A doctor may request urine metadrenalines when a person has persistent or recurring hypertension along with symptoms such as headaches, sweating, flushing, and rapid heart rate. They may also be requested when a person has hypertension that is not responding to anti-hypertensive treatment. Since the hormone production from a phaeochromocytoma is not regulated by the body, hypertension due to a phaeochromocytoma is frequently resistant to conventional therapies.
Occasionally, the test may be requested when an adrenal mass/lump is detected incidentally, on a scan done for another purpose (called an adrenal incidentaloma), or when someone has a family history of phaeochromocytomas. It also may be used as a monitoring tool when a person has been treated for a previous phaeochromocytoma.
-
What does the test result mean?
Because the urine metadrenalines test is sensitive to many outside influences and phaeochromocytomas are rare, a doctor may see more false positives with this test than true positives. If a symptomatic person has large amounts of metadrenaline and/or normetadrenaline in their urine, further investigation is indicated. If there are no interfering substances or stresses identified, then there is a good possibility that they may have a phaeochromocytoma. The doctor may request plasma metadrenalines to help confirm the initial findings. If these are also elevated, then imaging tests such as an MRI (magnetic resonance imaging) may be requested to help locate the tumour(s).
Serious illnesses and stresses can cause moderate to large temporary increases in metadrenalines. Doctors must evaluate the person as a whole – their physical condition, emotional state, medications, and diet. When interfering substances and/or conditions are found and resolved, the doctor will frequently re-test the person to determine whether the metadrenalines are still elevated. If they are, then they may request imaging scans; if they are not, then it is unlikely that the person has a phaeochromocytoma.
If metadrenalines are elevated in someone who has had a previous phaeochromocytoma, it is likely that, either treatment was not fully effective or, the tumour is recurring.
The ability of this test to rule out the presence of a phaeochromocytoma (negative predictive value of the test) is relatively good. This means that if metadrenaline and normetadrenaline concentrations are normal, then it is unlikely that a person has a phaeochromocytoma.
-
Is there anything else I should know?
While metadrenaline testing can help detect and diagnose phaeochromocytomas, it cannot tell the doctor how big the tumour is, where it is, how many tumours are present, or whether or not the tumour(s) are benign (although most are). Even small tumours can produce large amounts of catecholamines.
It is very important to talk to your doctor before discontinuing any prescribed medications. Your doctor will work with you to identify interfering substances and drug treatments to determine which of them can be safely interrupted and which must be continued for your well-being. Some of the substances that can interfere with metadrenaline testing include: paracetamol (acetaminophen), aminophylline, amphetamines, appetite suppressants, coffee, tea, and other forms of caffeine, chloral hydrate, clonidine, dexamethasone, diuretics, adrenaline, alcohol (ethanol), insulin, imipramine, lithium, methyldopa (Aldomet), MAO (monoamine oxidase) inhibitors, nicotine, nitroglycerine, nose drops, propafenone (Rythmol), reserpine, aspirin (salicylates), theophylline, tetracycline, tricyclic antidepressants, and vasodilators. The effects of these drugs on metadrenalines testing will be different from person to person and are often not predictable.
-
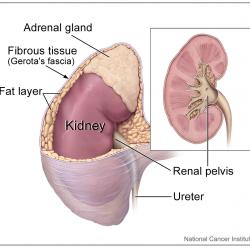
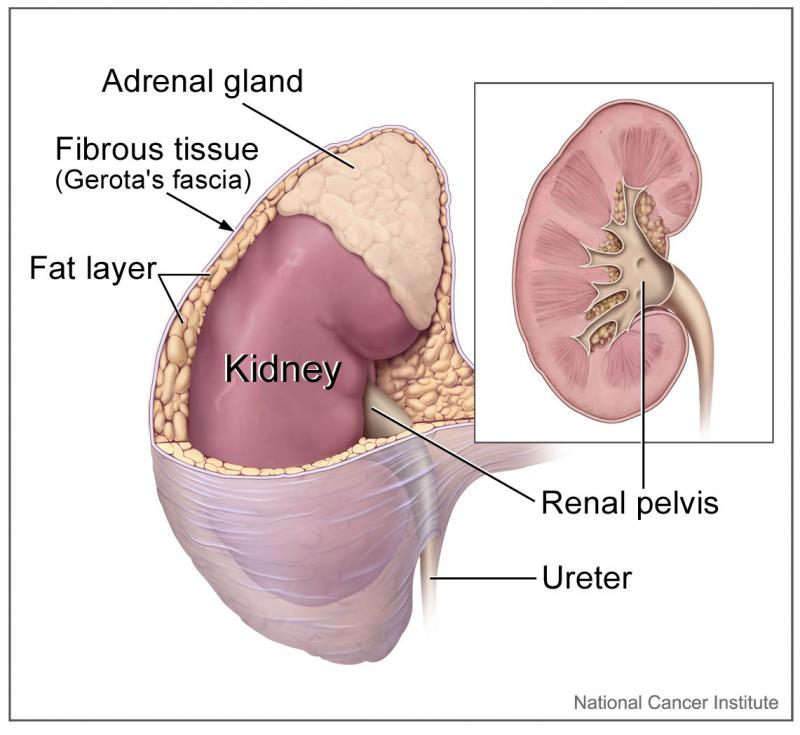
Can I have tumours in both of my adrenal glands?
Yes. Usually a single adrenal tumour will arise in one gland or the other, but multiple tumours can form. This is more likely in people with a strong family history of phaeochromocytomas.
-
If I avoid all of the interfering substances mentioned, could I prevent a phaeochromocytoma?
-
Why haven't I heard about phaeochromocytomas?
Because they are rare. They are important to diagnose, however, because they are a potentially curable cause of hypertension.
-
Will my doctor ever test for HVA or VMA?
Rarely, these tests have largely been replaced by measurement of urine and plasma metadrenalines. The latter tests should give your doctor the information they need. HVA and VMA are more useful in the diagnosis of other neuroendocrine tumours like neuroblastoma. Most phaeochromocytomas do not produce dopamine or HVA.
-
Is it really necessary to collect urine for 24 hours?
Yes, for accurate test results it is essential that all of the urine be collected. Because catecholamines are released at varying times, the one sample not included might be the one with the most metadrenalines in it. You may be asked to collect more than one urine sample; this increases the chances of including an episode of increased catecholamine production.